
POST-PARTUM DEPRESSION (PPD)
Postpartum Disorders
Postpartum disorders refer to mental health conditions that some mothers may experience after giving birth. However, not all new mothers will face these challenges. The development of postpartum disorders often depends on various factors, including individual circumstances and surroundings. Common types of postpartum disorders include postpartum depression (PPD), postpartum anxiety, postpartum blues, postpartum psychosis, postpartum hemorrhage, and postpartum infections.
Symptoms of Postpartum Depression (PPD)
The signs and symptoms of postpartum disorders can vary in severity, but some common indicators include:
• Severe mood swings
• Changes in appetite or eating habits
• Loss of interest or enjoyment in activities
• Difficulty sleeping and constant worry about self or the baby
• Pain or discomfort in the lower abdomen
• Excessive crying
• Hallucinations, delusions, or confusion
It’s important to recognize these symptoms early, as they may significantly impact both the mother and her ability to care for the baby.
Treatments for Postpartum Disorders
The first step in managing postpartum disorders is reassurance – understanding that help is available and that no mother is alone in this experience. Treatment approaches may vary based on individual needs, but some effective methods include:
• Counseling and Therapy: Cognitive-behavioral therapy (CBT) and other therapeutic approaches can help reduce symptoms and improve mental well-being.
• Self-Care: Maintaining regular physical activity, a balanced diet, and sufficient rest are essential for managing postpartum disorders.
• Supportive Relationships: Open communication with family members, especially partners, can foster understanding and strengthen relationships, contributing to quicker recovery.
Seeking professional help from mental health providers specializing in postpartum conditions is crucial. At Hapinus Care centers in Trivandrum and Kozhikode, we offer expert guidance and compassionate care to support mothers during this challenging time.
BIPLOAR DISORDER
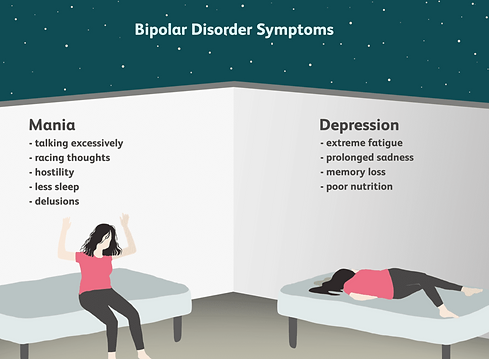
Bipolar disorder is a mood disorder involving dramatic shifts in mood, energy, and activity levels that can disrupt daily life. These shifts include:
• Manic episodes: Periods of elevated mood, increased energy, reduced need for sleep, racing thoughts, and impulsive behavior.
• Depressive episodes: Periods of low energy, sadness, loss of interest in activities, fatigue, and thoughts of hopelessness.
It is categorized into different types, including Bipolar I, Bipolar II, and Cyclothymic Disorder, depending on the severity and duration of mood episodes.
Borderline Personality Disorder (BPD)
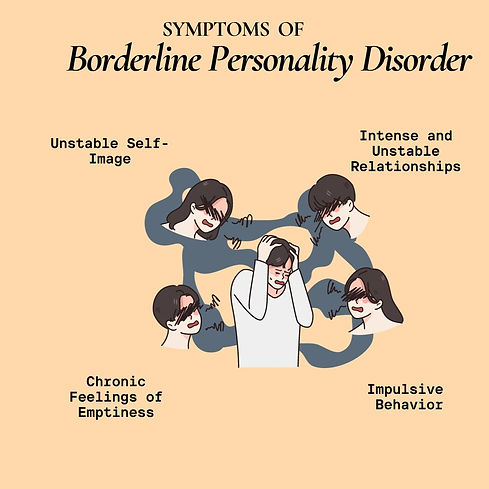
BPD is a personality disorder characterized by pervasive patterns of emotional instability, self-image issues, and difficulty maintaining relationships. Key features include:
• Intense fear of abandonment.
• Impulsive and self-destructive behaviors (e.g., substance abuse or self-harm).
• Unstable interpersonal relationships, alternating between idealization and devaluation.
• Chronic feelings of emptiness and intense, often inappropriate anger.
• Episodes of dissociation or paranoia under stress.
It often stems from a combination of genetic, neurological, and environmental factors, such as early trauma.

Behavioral Problems in Children
Behavioral problems in children refer to persistent disruptive or inappropriate behaviors that interfere with their social, academic, and family life. Common issues include:
• Oppositional Defiant Disorder (ODD): Frequent anger, irritability, defiance, and hostility towards authority figures.
• Conduct Disorder (CD): Aggressive behaviors, lying, theft, and violation of rules or others’ rights.
• Attention-Deficit/Hyperactivity Disorder (ADHD): Difficulty focusing, hyperactivity, and impulsivity.
Behavioral problems can arise due to genetic, psychological, or environmental factors, and early intervention can significantly improve outcomes.
Obsessive-Compulsive Disorder (OCD)
OCD is an anxiety disorder involving recurrent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to reduce distress or prevent a feared outcome.
• Obsessions: Persistent and unwanted thoughts, fears, or urges, such as fear of contamination or harm.
• Compulsions: Ritualistic behaviors or mental acts, such as excessive cleaning, checking, or counting.
These symptoms can be distressing, time-consuming, and interfere with daily functioning.


Obsessive-Compulsive Personality Disorder (OCPD)
OCPD is a personality disorder where individuals are preoccupied with orderliness, control, and perfectionism, often to the detriment of flexibility and efficiency.
Key characteristics include:
• Rigidity in following rules and schedules.
• Reluctance to delegate tasks or collaborate due to fear that others won’t meet their standards.
• Excessive devotion to work at the expense of leisure and relationships.
• Difficulty discarding objects, even when they have no value (hoarding).
Unlike OCD, individuals with OCPD do not typically see their behavior as problematic.
Psychosis
Psychosis is a symptom, not a disorder, involving a loss of connection to reality. It is often seen in conditions like schizophrenia, bipolar disorder, or substance-induced psychosis. Symptoms include:
• Hallucinations: Experiencing things that aren’t real, such as hearing voices or seeing things that aren’t there.
• Delusions: Strongly held false beliefs, such as paranoia or grandiosity.
• Disorganized thinking and speech: Incoherent thoughts or difficulty following a conversation.
Psychosis may be caused by a mix of genetic, biochemical, and environmental factors.

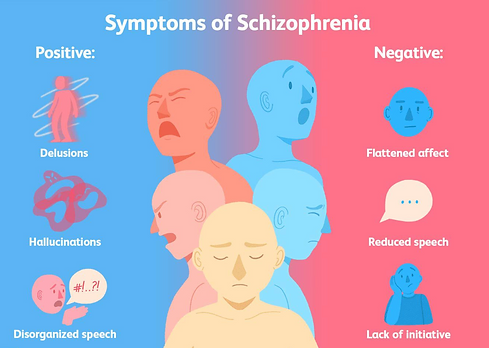
Schizophrenia
Schizophrenia is a chronic and severe mental disorder that affects how a person thinks, feels, and behaves. It is marked by episodes of psychosis and ongoing impairments in functioning.
Core symptoms include:
• Positive symptoms: Hallucinations, delusions, and disorganized speech or behavior.
• Negative symptoms: Reduced emotional expression, lack of motivation, and social withdrawal.
• Cognitive symptoms: Impaired attention, memory, and decision-making abilities.
Schizophrenia typically emerges in late adolescence or early adulthood and requires a combination of medication, therapy, and support to manage.
